Spinal Injections (and Sciatica vs Sacro Iliac pain)
Question: I have terrible pain in my lumbar spine. My medical doctor recommended I see a Spine Doctor. Two MRI’s, showed bulging discs and curvature in my spine. He recommended spinal injections. After two, I was still in pain, so he asked me to come back for one more injection. While I was lying face down and supposed to be sedated mildly he injected the needle into my lumbar. I could feel the pain shooting down the back of what has always been my “stronger” leg. I've have been having shooting pain in that leg every day, since last October when I received the injection. I'm diabetic and these shots ran my sugar up. I’m very discouraged.
Reply: The above letter brings up the common issue of back pain combined with radiating leg pain. In a future article I hope to discuss specific clinical issues including how to differentiate Sciatica (nerve root impingement by a disc) from Sacro Iliac joint – both can cause back pain and leg pain. In this article, I thought it would be helpful to remark on a few key phrases and words in the letter that might be helpful to readers in similar situations. These may reflect some common patient misperceptions and therefore present the opportunity for education.
“Spine Doctor” In actuality, multiple different specialties can focus on management of spine problems. These can include surgeons such as neurosurgeons or orthopedists. Sports medicine physicians, rheumatologists, rehabilitation physicians, and primary care physicians can all develop practices that focus on the spine. Additionally, physicians that perform spine injections can include anesthesiologist, neurologists, and rehabilitation physicians. Any of these physicians may be Board Certified in Pain Medicine but their background training specialty reflects how they approach patient care. In my opinion, it is important to research a physician before a visit to know the background of the person making the recommendations. Of the three specialties, a rehabilitation physician is much more likely to look at the biomechanical issues in polio patients and how this contributes to pain. To find a rehabilitation physician, check out the Physician Finder under the “About Physiatry” tab at aapmr.org. On the other hand, if a spinal injection is clearly indicated then anesthesiologists and neurologists are certainly more than competent at providing that service.
“Bulging Discs” In actuality, bulging discs are extremely common and often are incidental findings that may cause no symptoms. If disc disease progresses and there is actual disc herniation on an MRI scan, the findings MAY be the cause of pain radiating down the leg (if the disc is pressing on a nerve with distribution that correlates to the pain). It is very common to see reports with nerve compressions on the opposite side or at a different level than the reported pain – those findings often need to be ignored. In a similar way, disc extrusions (when the disc material has disconnected from the disc space) may or may not correlate with the clinical area pain. In my experience, many patients are told the results of an MRI scan and immediately assume findings are the cause of pain, while the same findings could be found in a high percentage of people walking the street with no symptoms at all.
“Spinal injection” There are actually a number of different types of spinal injections and patients should ask enough questions that they understand exactly what procedure is going to be performed. I suggest bringing a friend or family member as well as a notepad to appointments and writing down the exact procedure being proposed. It is rather amazing to me that so many individuals will allow a physician to stick a long needle in the back without clearly understanding where the needle is going.
Facet injections address the small joints between spine segments when they become arthritic.
“Nerve blocks” or “rhizotomy” procedures can also be performed for facet problems.
In the treatment of discs causing nerve impingement, Epidural Steroid Injections (ESI) are often done in a series of three.
If there’s no response to the first two, the third injection is usually not provided.
ESI can help avoid surgery while dramatically improving pain and function in appropriately selected individuals.
The procedure is safe and the epidural injection is the same one typically used during childbirth (with different medicine).This should say something about the overall low risk. I would not hesitate to have one myself, if indicated, since the long-term risks of pain/immobility can exceed the risk of the procedure.
Having said that, the question above could reflect transient injury to spinal nerve during the procedure which is a known but rare complication.
At the same time, ESI procedures are often recommended without clear indications. If the recommendation is made but the reasoning does not completely “add up” then a second opinion is suggested. As outlined below, the sacroiliac joint is a common source of pain in Polio survivors that can mimic nerve root irritation by a disc.
Steroids certainly can raise blood sugar in diabetics. This is typically brief and not problematic unless individual has had control blood sugars to begin with. This should be discussed with one’s primary care physician and not presumed to be a problem.
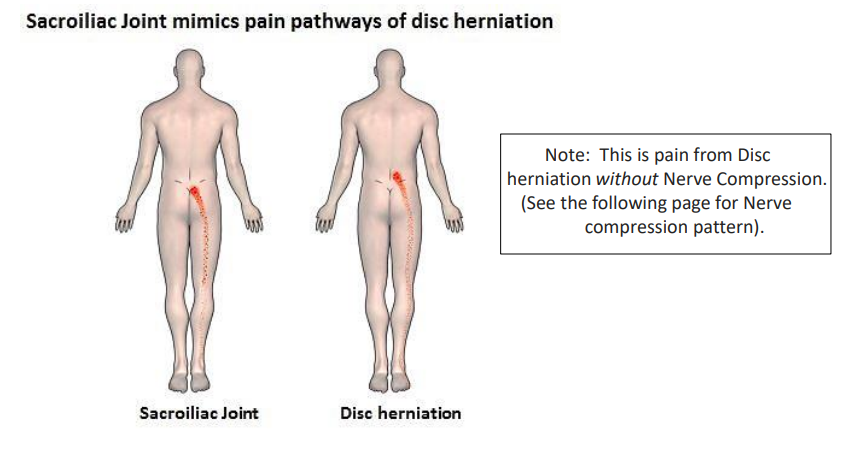
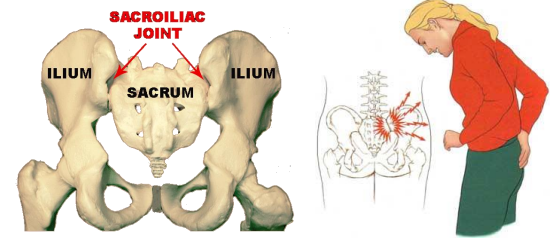
Lastly, it is important to understand that a good rehabilitation physician can differentiate between back/leg pains due to a disc causing nerve impingement (“Radiculitis” or “Sciatica”) as opposed to pain coming from the Sacro Iliac Joint. The latter is extremely common in polio survivors due to the fact that muscle weakness/imbalance, gait abnormalities, and differences in leg length put enormous stress on that joint. As noted above, this is the subject for another article however some differences are noted below.
“Sacro Iliac” pain starts a bit lower than Disc Herniation pain. BOTH cause pain down into the buttocks and leg.
Sacro Iliac pain is due to the SI joint. Pain can be constant or it can come and go as the joint is stressed. Sometimes there is “popping” in and out of place.
When disc herniation causes “Sciatica” (and presses on the L5 or S1 nerve roots that merge into the Sciatic nerve) the pain usually goes all the way to the foot.
Please watch for future articles where we will hope to discuss the above further and address other treatment options. While both Sciatica and Sacro Iliac pain can be appropriately treated with injections, there are many other approaches which should first be considered including exercises and changes to how one sits and walks.