Concepts of Shoulder Self Management for the Polio Survivor
We recently published an article titled “Shoulder Problems in Polio Survivors”, which talked about common shoulder diagnoses. This article will focus on some key approaches to self-management. Clearly any shoulder rehabilitation program needs to start with a specific diagnosis (reviewing an individualized exercise program is far beyond the scope of this article). I hope to explain some basic approaches that may encourage polio survivors to understand that relief of shoulder pain is possible.
Any persistent shoulder pain should be evaluated by an appropriate healthcare provider and I would highly suggest requesting a specific home exercise program to supplement any other treatment.
I will review some basic physiology concepts regarding the shoulder, which your health care provider will take into account when determining your specific exercises.
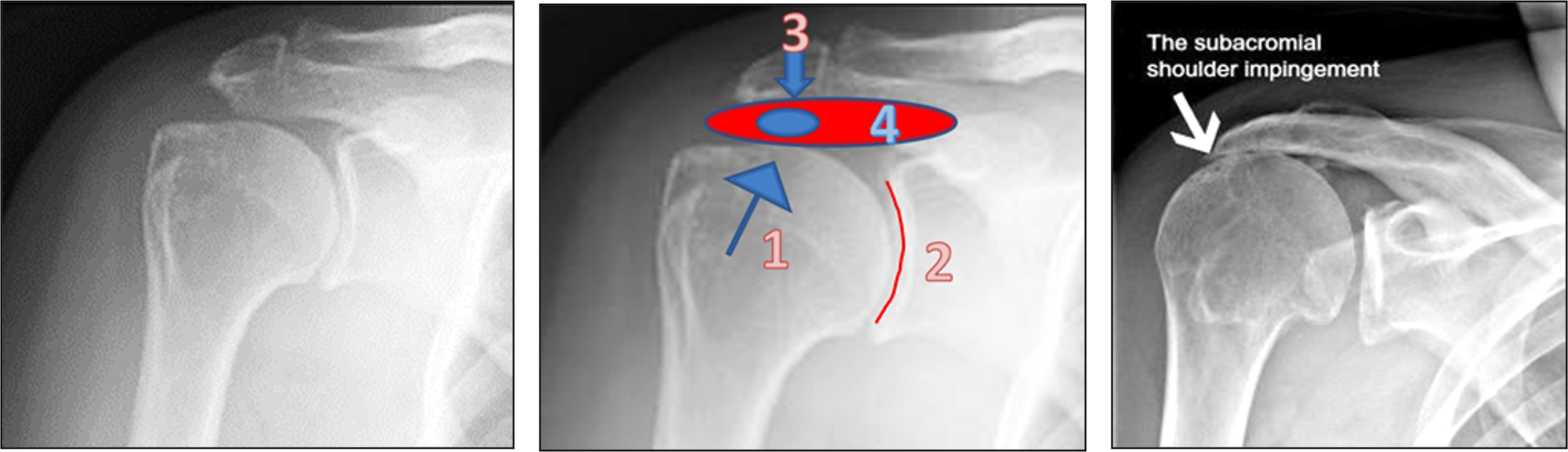
The shoulder is inherently unstable with the “ball” (#1 in graphic on the next page ) of the humerous (upper arm bone) fitting into a very shallow “cup” (#2) of the shoulder blade (scapula). It is the muscles, tendons, and ligaments that keep the shoulder in place.
Muscle weakness can cause excess motion within the shoulder joint, leading to increased pain and long-term problems such as tendinitis and arthritis.
Strengthening muscles that bring the humerus (#1) down in the shoulder joint during movement can be essential part of rehabilitation. Your physician or therapist may mention the “Supraspinatus”, “Infraspinatus”, or “Teres Minor” (together called the “external rotator” muscles) when discussing this. Another rotator cuff muscle (the Subscapularis) is in the underside of the shoulder blade. Together these muscles are the key to shoulder stability.
Muscle tightness can also alter the normal motion of the humerus within the shoulder joint.
Heat and cold both have therapeutic benefit.
Moist heat is often helpful prior to stretching or activity in order to loosen tissues.
A cold pack can be very helpful after activity, to relieve muscle spasm, or to reduce inflammation. One only has to watch a professional pitcher in the dugout after he pitches to understand that ice can prevent inflammation and pain after activity. A pitcher routinely uses a bag of ice on the shoulder for this purpose to require less recovery time prior to his next game. I often say, “if it is good enough for a million-dollar pitcher, it should be good enough for all of us”.
Nonsteroidal anti-inflammatories can also be helpful if taken regularly for 7 to 10 days. They should always be taken with food and discontinued if there is G.I. upset. Individuals with kidney disease or other medical problems should only take these under the direction of a physician. While many people are hesitant to take medications, a reduction in the inflammation of the shoulder and restoring normal function can actually prevent further damage and have benefit far after the medication is discontinued. This is very different than taking medications such as “painkillers”.
The concept of “impingement” is very important in understanding the shoulder. In the above diagram the humerus (#1) can ride up in the shoulder joint and “impinge” the rotator cuff (#4) against the part of the shoulder blade: the acromion (#3). This can produce tendinitis of the rotator cuff muscle or even a tear (indicated by a blue oval). Impingement is especially problematic if the acromion (#3) does not have a flat under surface. Often a “hook” (sharp protrusion of bone pointing down) can exist causing increased damage in the tendons when the humerus rides up. Because of this phenomenon, it is essential that rotator cuff muscles function as normally as possible and prevent the humerus from elevating when the shoulder moves.
Posture of the spine can be essential in preventing shoulder damage. The under surface of the acromion (#3) should be horizontal to the ground when we are standing or sitting. If we do not “sit tall” with a good curve in the low back then the shoulders become “rounded” and the acromion (#3) is no longer horizontal to the ground but rather tips forward narrowing the space for the rotator cuff (#4).
There is no question that issues such as weakness around the shoulder and posture are more problematic in the Polio population. I am always aware of this when determining the need for a power vs manual wheelchair. Rather than this being a reason to “live with” shoulder pain, I see it as a reason to more aggressively seek assistance (sometimes lifelong) to optimize shoulder biomechanics and minimize the long term impact on function. Rehabilitation physicians, Physical Therapists, Orthopedists, and even many primary care physicians can have the knowledge to help.
As always, it is important to find the health care provider that will listen to your unique circumstances and “have the heart of a teacher” to share with you specific individualized approaches. This kind of care can help maintain your shoulder integrity over the years.