Arthritis and the Knee - What are my Options?
Question: I have arthritis and some bone spurring in my weak left leg. The pain has been unbearable. I had a cortisone shot in my knee, which helped with the pain. How does or will it, affect my polio leg? What are your thoughts on orthoscopic surgery or replacement of the knee.
Answer: Your question is a common one and is a good example of how a typical problem (arthritis) can be much more problematic for a Polio survivor.
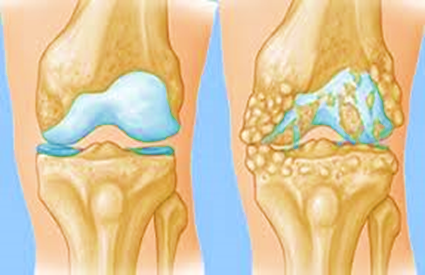
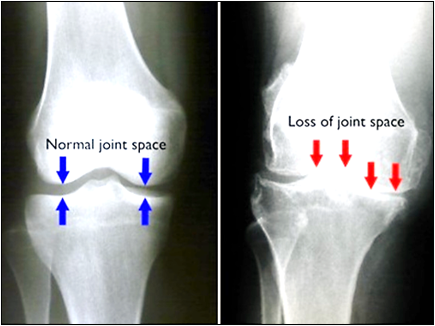
First off, we should define arthritis. Any word beginning with any version of “arthro” refers to a joint. The end of the term, “itis” means inflammation. So, arthritis is literally joint inflammation. The inflammation can be due to many causes and include immune diseases such as rheumatoid arthritis. The most common cause is osteoarthritis, also called degenerative arthritis, in which joint wear and tear is the focus. In degenerative arthritis the normal smooth surfaces of the joint have become worn and expose rough bone. The rough surfaces rubbing on each other create an inflammatory cascade that can cause further joint destruction and lead to abnormal bone growth such as bone spurs. A healthy joint resembles the joint you would see in carving a chicken or turkey with white/smooth surfaces that fit together nicely.
A severely arthritic joint can have a dramatically different appearance and loose the biomechanical effect it was originally designed to have. As a result, there can be pain from the inflammation and a level of instability that results in functional impairment. In the case of the knee, this often leads to a decrease in ambulation. Unfortunately, decreased activity leads to deconditioning and the loss of muscle strength leads to abnormal movements of the joint and more instability. A cycle is established where inflammation causes pain. Pain causes reduced activity. Reduced activity causes weakness. Weakness causes instability and then more inflammation.
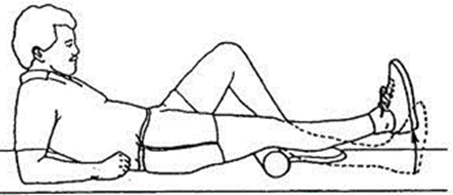
Whenever possible, it is important to try to interrupt this cycle. This may include learning exercises that strengthen the knee muscles with out causing pain (e.g. isometric “Quad Sets”) or using non-steroidal anti-inflammatory medications (NSAIDS). Anti-inflammatory medications have gotten a bad rap in recent years due to potential adverse effects. This should be discussed with your doctor. I generally recommend against long term NSAIDS in favor of taking them at full dose for 10 to 14 days then stopping. This minimizes the chances of adverse effects while maximizing the potential benefit. Another option is an oral steroid as an anti-inflammatory, but this should be used very sparingly and rarely repeated due to multiple potential problems highly correlating with long term steroids. Steroid injections into the knee can provide the benefit with some reduction in the long term risks. In my opinion, injections should always be done in conjunction with Physical Therapy or a regular home exercise program. As one weighs risks and benefits of oral or injected anti-inflammatory medications, it is important to weigh the risk of not treating and having disease progression as well as the potential benefit that short term treatment to control inflammation can allow therapy or home exercises to rebuild strength and therefore joint stability. Improved joint stability and biomechanics then reduces the chance of inflammation reoccurring. It is important to remember that permanent destructive changes do occur in the joint, but many other factors are at play. It is not uncommon for someone to have no pain one week and start with significant arthritis pain the next. Typically, the joint did not deteriorate overnight. Rather, the other factors including reduced muscle stabilization led to a point where a relatively mild trauma, such as overuse, kicked off the above cascade. In some cases, this can be undone and years of relatively pain free function can follow.
While the above is true, it is a very big challenge in an individual with Polio to improve muscle stabilization in a knee on their weak leg. Sometimes appropriate bracing of the foot and ankle can dramatically change the stress on the knee and thereby reduce knee pain. Bracing of the knee itself is less helpful but can provide some short term relief for some individuals. While bracing the foot and ankle can provide long term improvements in biomechanics for some individuals, bracing of the knee itself does not really alter the underlying biomechanics.
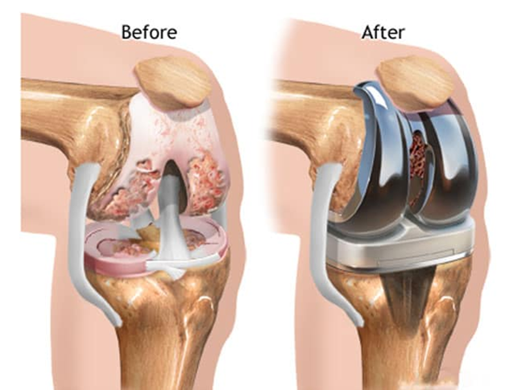
If therapy/home exercises, bracing and anti-inflammatory medications do not work, surgical intervention is reasonable to consider. Arthroscopic surgery had been very common in years past to “clean out” degenerative tissue in an arthritic knee. Studies have shown that most of those surgeries did not change outcome. Still, there is a role for arthroscopic surgery if specific lesions are present and pain reduction can be dramatic in these cases. This is an option to consider if offered by the orthopedist. At the same time one should carefully discuss the “down time” post operatively and resultant problems that may create for the Polio survivor. Similarly, total knee replacement surgery can have profound benefits for some but needs to be planned carefully and specific individualized risks discussed with the surgeon.
Typically, joint deformity in a severely effected Polio knee is significant and I would suggest having a couple of opinions to discuss options. Usually, a prosthetic knee that has more than the usual internal stability is selected. A detailed discussion of Total Knee Replacement in Polio is beyond the scope of this short article. My overall recommendation would be to proceed slowly, don’t be afraid, but be wise and ask lots of questions. Joint replacement can be life changing, it can also backfire and worsen disability.