Immunizations are for Everyone: Not Just for COVID and Not Just for Kids
World Immunization Week is celebrated every year during the last week of April. In 2023 that will be April 24-29. The purpose is to highlight the collective action that is needed to emphasize the critical need for vaccination and to promote the use of vaccines (immunizations) to protect people of all ages against serious disease. The ultimate goal is for community acceptance so that more people will be protected from vaccine-preventable diseases.
We, polio survivors, have seen first hand the value of polio vaccines that were first released to the public in the U.S. in 1955 (killed virus - Salk/injectable) and in the early 1960s (live, attenuated - Sabin/oral) and the subsequent sharp decline in the number of people paralyzed by polio. And, we have seen a significant drop in the number of people who have gotten seriously ill, possibly needing a ventilator to help them breathe, or have died since COVID vaccines became available.
Smallpox was the first human infectious disease ever eradicated and that, was a direct result of one thing - Vaccination.
How many of us have known a child who has died of tetanus or diphtheria? I suspect none! Those of us in our 50s or older do remember getting sick with measles, mumps, and/or chickenpox. But young people today hardly ever get sick or miss days/weeks of school because they have one of these diseases. This is because, since the 1970s, the majority of children are protected from these diseases by immunizations. In fact, if children are fully immunized by the time they start first grade, they will have received between 17 and 29 immunization shots. The number of injections depends on how many of the immunizations combined 2 to 4 vaccines into one injection. Some health insurances will cover the cost of combo vaccines and some will not; some facilities stock the combo vaccines and some do not.
Once individuals finish attending school, and hence have no school nurse monitoring immunization records, immunizations tend to be forgotten and neglected. There are no regular immunizations recommended for adults aged 26 through 50, other than once every 5 to 10 year boosters against tetanus and recommendations for annual flu vaccines (and whatever the COVID vaccine schedule is going to be).
However, as a person approaches their 50th birthday and beyond, recommendations for vaccines again appear. Certain health conditions, occupational exposures, or travel overseas may also dictate the need for certain vaccinations or a different vaccination schedule.
Current Vaccines Recommended for Adults Over Age 50 :
Annual flu vaccines and what may likely be annual COVID vaccines.
One dose of Tdap (Tetanus, diphtheria, activated pertussis/whooping cough) and then Tetanus/Diphtheria or Tdap booster every 10 years
People often call tetanus “lockjaw” because one of the most common signs of this infection is tightening of the jaw muscles.
Diphtheria is a serious illness that spreads easily. Doctors treat it immediately and aggressively. Doctors first ensure that the airway isn't blocked or reduced. In some cases, they may need to place a breathing tube in the throat to keep the airway open until the airway is less inflamed. (1)
Tetanus infection can lead to serious health problems, including being unable to open the mouth and having trouble swallowing and breathing. (2)
Shingles vaccine - series of two injections of Shingrix once in lifetime.
Current Vaccines Recommended for Those Age 65 or Older (or younger with certain risk factors):
Annual flu vaccines and what may likely be annual COVID vaccines.
Pneumococcal vaccines (PCV 15, PCV 20, or PPSV23). The vaccination schedule has changed several times since 2000.
In 2023 the recommendation is one dose of PCV15 (Vaxneuvance) followed by PPSV23 (Pneumovax)
Or a single dose of PCV 20 (Prevnar 20)
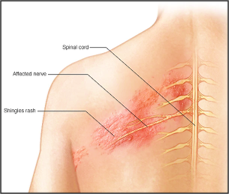
Shingles (medical term: herpes zoster) is produced by a reactivation of the varicella-zoster virus that causes chickenpox. It happens most often in people over 50 and in those who experienced the painful, itchy skin lesions from having had the disease chickenpox.
The CDC describes what it feels like to have shingles:
“The rash is usually painful, itchy, or tingly. These symptoms may precede rash onset by several days. Some people may also have headache, photophobia (sensitivity to bright light), and malaise in the prodromal phase.
The rash develops into clusters of vesicles (small blisters). New vesicles continue to form over three to five days and progressively dry and crust over. They usually heal in two to four weeks. There may be permanent pigmentation changes and scarring on the skin.” (2)
The Shingles rash is usually along the course of one or two adjacent paths of the involved nerves anywhere on the body is seen most often on the trunk, and characteristically does not cross the midline of the body.
It’s important to note: this virus is NOT the same as the virus causing genital herpes!
Some people develop post-herpetic neuralgia that can cause unrelenting pain in the area that showed the outbreak of skin lesions. This can last for months, years and in the worst cases, become permanent. There are some medications that can help but they are not 100% effective and are not curative.
Ophthalmic shingles (Shingles in the eye) is one particular version of the disease that can have some serious side effects, that ultimately can cause permanent damage to your vision. (1)
Shingles can affect the facial nerve near one of your ears (Ramsay Hunt Syndrome). In addition to the painful shingles rash, Ramsay Hunt syndrome can cause facial paralysis and hearing loss in the affected ear.
Many people complain about a sore arm after the 2 dose shingles vaccine. That’s minor compared to the pain this virus can bring.
Pneumonia is a generic term for any infection that inflames the air sacs in the lungs. Pneumonia can be caused by viruses (such as influenza and COVID) along with many different bacteria, and fungi.
Symptoms can range from relatively mild to life-threatening. It is most serious for infants and young children, people over 65, and individuals with various health problems and immune system disorders.
Pneumonia is often classified depending on the likely place where/how the person got the infection. Thus, you can hear these terms to describe it:
“Community-Acquired Pneumonia (CAP)” and “Healthcare-Acquired Pneumonia” (HCAP). CAP generally affects relatively healthy people and is usually treated with common antibiotics: HCAP is more likely to be resistant to one or more antibiotics and the people who get it are usually already sick with other conditions.
Aspiration pneumonia occurs when food, drink, and/or saliva or vomit is inhaled into the lungs.
The vaccines that can decrease a person’s risk of getting pneumonia are the flu shot, the COVID vaccine, and the various pneumococcal vaccines. However, getting one of the pneumococcal vaccines will NOT prevent all pneumonias.
It will not prevent pneumonia from bacteria that are not pneumococci (streptococcus pneumonia) such as the bacteria causing Legionnaires’ disease, or bacteria-like organisms such as Mycoplasma, viruses, or fungi.
And it will not prevent the damage caused to lung tissue caused by aspiration of bacteria that are present in the mouth or stomach acid.
Of Importance to note: The vaccines for COVID, Flu, Shingles and Whooping Cough do decrease your risk of getting these diseases but do not prevent you from getting it. The purpose of these recommended immunizations is:
To prevent serious disease, hospitalization (and death from Flu and COVID);
To minimize the risk of adults becoming ill from whooping cough when exposed to it, and to lessen the transmission of the whooping cough bacteria to infants/young children who are too young to be fully protected by immunizations;
To prevent the pain and suffering that comes with an episode of herpes zoster, known more commonly as “shingles”,
To decrease the number of episodes and risk of hospitalization from pneumonia, and minimize the damaging effects caused by the pneumococcal bacteria.
Please talk to your primary care physician about staying up to date on the vaccines YOU may want or need.
Sources:
(2) www.CDC.org
(3) Cleveland Clinic